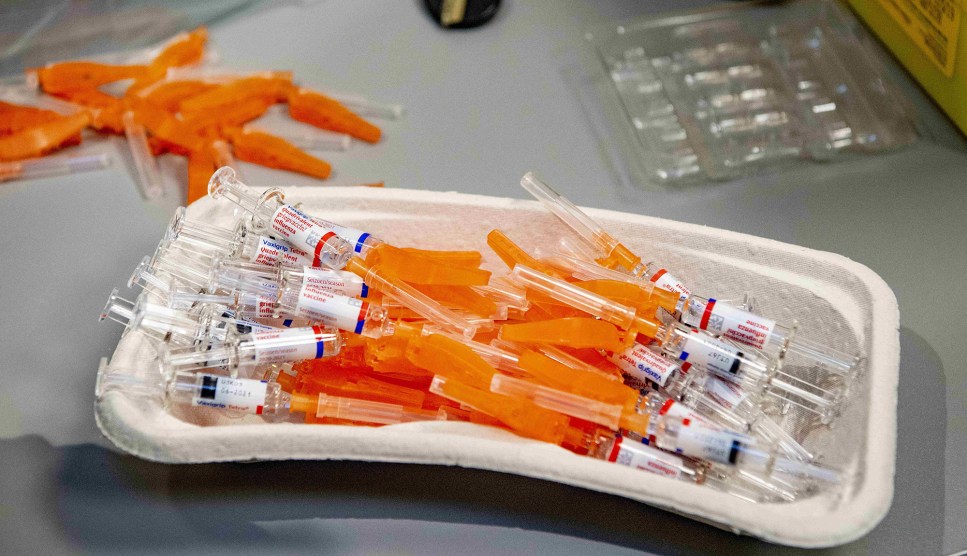
Mario Tama/Getty
As many as 40 million doses of two COVID-19 vaccines are expected to be available for distribution by the end of December—enough to vaccinate 20 million people. But in a country of more than 330 million, who should be the first in line to get them?
Yesterday afternoon, a panel of expert advisors to the Centers for Disease Control and Prevention voted 13 to 1 to recommend that health care workers and residents of long-term care facilities get top priority for vaccination. That group would include about 20 million medical providers, EMTs, home health aides, pharmacists, and nursing home staff, as well as the roughly 3 million people who live in skilled nursing and assisted living facilities.
The idea behind vaccinating health care workers first is to protect the people who keep the health care system running, many of whom are at risk of exposure to the coronavirus while on the job. Residents of long-term care facilities, meanwhile, are considered the most at-risk populations, accounting for about 40 percent of all US coronavirus deaths despite making up less than 1 percent of the population.
While individual states will have the final say on who gets the vaccines first, they are expected to follow the recommendations of the panel, known as the Advisory Committee on Immunization Practices. Making these decisions has become even more urgent as the numbers of new cases and hospitalizations have soared to record levels in the past month. “Since we’re averaging one COVID death per minute in the United States right now, in the time it takes us to have this ACIP meeting, 180 people will have died from COVID-19,” said Beth Bell, chair of the panel’s COVID-19 vaccine work group, at the start of Tuesday’s meeting. “So we are acting none too soon.”
Arkansas Secretary of Health José Romero, the committee’s chair, said the recommendation reflects the principles of “maximum benefit, minimum harm” and mitigates inequalities in vaccine distribution. Kathleen Dooling, a CDC medical officer, explained that the choices “promote justice” because health care personnel put themselves at risk to care for patients during the pandemic, and because all long-term care facilities are expected to get access to vaccines at about the same time, regardless of their patients’ socioeconomic status.
The committee is made up of medical and public health experts who issue recommendations on all kinds of vaccinations, from flu shots to childhood inoculations. Since the spring, it has been studying and discussing the scientific, ethical, and practical questions of who should get priority for COVID-19 vaccines once they are available. The committee is considering recommending that following health care workers and long-term care residents, vaccinations should be made available to essential workers such as teachers, agricultural workers, and police, followed by adults over 65 and people with high-risk medical conditions.
Meanwhile, the arrival of functional vaccines appears imminent. Pfizer and Moderna have both asked the FDA to issue emergency use authorizations for their vaccines, which are reported to be about 95 percent effective against the coronavirus. However, there are significant logistical challenges associated with each vaccine. Both require two doses spaced several weeks apart, and it may be difficult to track patients in nursing homes, where there can be frequent turnover among residents. Additionally, because some adults in the vaccine trials reported side effects including fever, headaches, and muscle pain after receiving their second dose, ACIP members discussed the need to stagger vaccinations for health care workers to avoid, for instance, an entire hospital unit calling in sick.
Despite these challenges, “most jurisdictions” in the county believe they will be able to vaccinate all health care workers within three weeks, Nancy Messonnier, the director of the National Center for Immunization and Respiratory Diseases, said at the meeting Tuesday. And nearly all skilled nursing facilities nationwide have enrolled in a program to receive vaccinations from CVS and Walgreens pharmacies.
“To all the people out there that are anxiously waiting for this vaccine,” Messonnier said, “we hope that this vote gets us all one step closer to to the day when we can all feel safe again, and when this pandemic is over.”