<a href="http://www.shutterstock.com/pic-166732214/stock-photo-doctor-on-the-phone.html?src=ZKaRmpeukcY4BzYMoKijTA-1-5" target="_blank">auremar</a>/Shutterstock
I’ve written before about the scary rate of antibiotic overprescription—so when a friend mentioned that she knew someone who had been prescribed antibiotics after his doctor evaluated him via Google Hangout, I was alarmed. Curious as to how common this practice was, I decided to do an informal survey of friends and colleagues. Their responses surprised me: While no one reported a similar Hangout antibiotics experience, most recalled describing conditions to their doctors via email or over the phone—and receiving a speedy response back that a prescription for antibiotics was waiting for them at the pharmacy.
One friend told me that because of her recurring urinary tract infections, she was grateful that her doctor was willing to give her antibiotics without seeing her. I could see her point: Why should she schlep all the way to her doctor’s office every time she feels an infection starting, only to have her doctor tell her what she already knows?
It’s hard to say how commonly doctors prescribe a patient antibiotics without an in-person visit; there isn’t much data on the practice, and there are no hard and fast rules governing it. In an email, a spokeswoman for the Centers for Disease Control and Prevention told me that the agency considers an examination necessary “to determine whether a patient likely has a bacterial infection to inform the provider whether an antibiotic is needed”—but the CDC leaves it up to the individual physician how he or she determines whether to prescribe an antibiotic. A spokeswoman for HMO giant Kaiser Permanente said that company doesn’t have rules about the practice, either. “A physician will make an assessment about whether or not to administer antibiotics over the phone or by secure message by taking into account the personalized needs of that patient,” she wrote in an email.
A 2013 study published in the Archives of Internal Medicine suggests that doctors are more likely to prescribe antibiotics when they don’t perform a physical evaluation. Researchers from the University of Pittsburgh School of Medicine found that people with symptoms of a urinary tract infection who had “e-visits”—where patients answer a series of questions about their conditions online instead of visiting their doctors’ office—were 50 percent more likely to get antibiotics than their counterparts who made office visits. E-visit patients with symptoms of sinusitis (which is usually caused by a virus, against which antibiotics are ineffective) were 5 percent more likely to get antibiotics than office visitors with the same symptoms.
Stuart Levy, a microbiologist at Tufts University’s School of Medicine and president of the Alliance for the Prudent Use of Antibiotics, believes that over-the-phone prescribing is common, especially for conditions with distinctive symptoms, such as urinary tract infections and children’s ear infections. In some cases, he says, the practice makes sense—say, if a doctor has seen a patient in person a few days earlier, and the symptoms haven’t cleared up, or for certain chronic conditions. But he says people often abuse the system. “Parents will stay up until midnight or later and then call the doctor and convince him to give them a prescription without seeing the kid in person,” he says.
In most cases, Levy says, the trek into the office is worth the trouble. A physical examination gives doctors much more information than a phone call or email; in person, the doctor can, for example, assess a person’s coloring, check for swollen glands, and palpate the belly. For patients who really don’t want to (or can’t) come into the office, both Levy and the CDC recommend a compromise: The doctor can write a prescription that the patient can fill in a day or two if symptoms don’t improve.
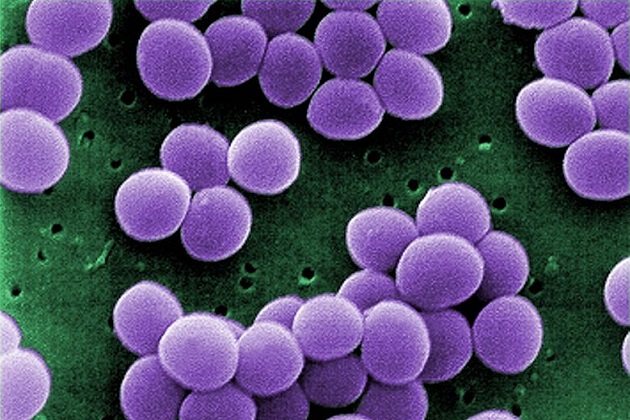
This method is common in Europe, but Levy says that so far, few American doctors have embraced it. They should, Levy says. I’m inclined to agree: Considering the growing number of antibiotic-resistant “superbugs,” the dearth of new drugs in the pipeline, and the high cost to our health care system of prescribing unnecessary antibiotics, it’s safe to say that these powerful drugs should be used as sparingly as possible.