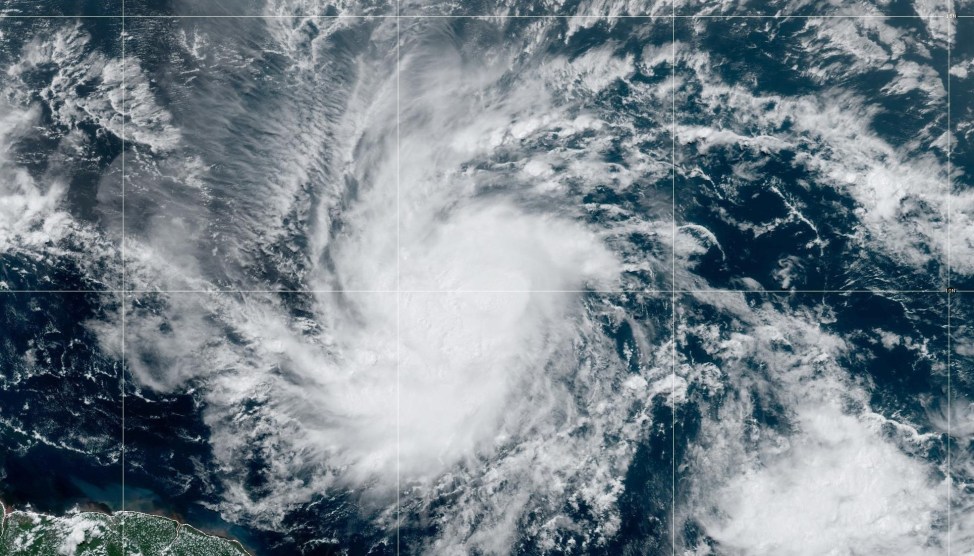
The emergency department of a hospital.Jonathan Torgovnik/Getty
This piece was originally published in High Country News and appears here as part of our Climate Desk Partnership.
Editor’s Note: The data here does not include all medical facilities and is a baseline look at hospital capacity based on available federal data. This story will be updated as we hear from locals who help fill in information gaps missing in the data.
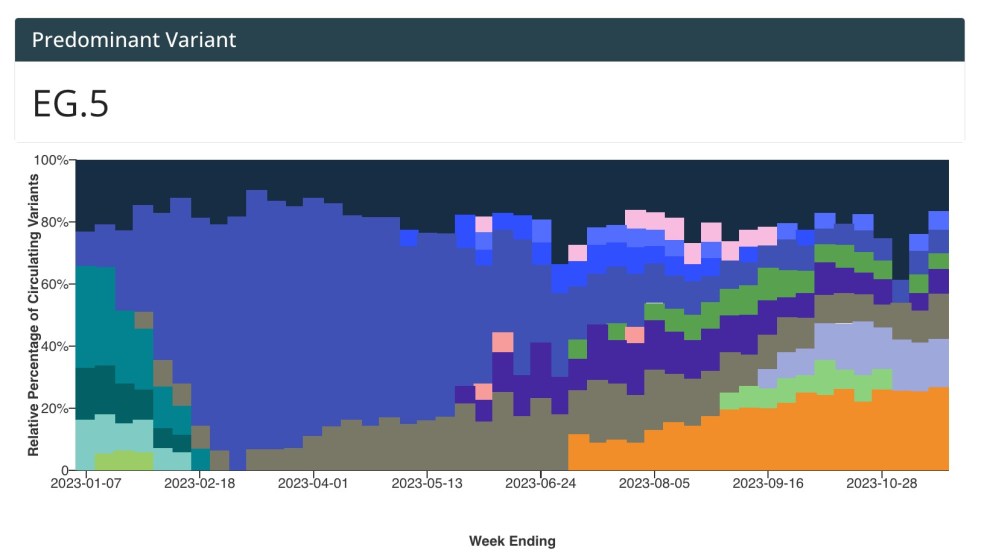
As the Western United States continues to see a rise in COVID-19 cases, it’s important to get a sense of the region’s health-care capacity. Identifying underserved areas and connecting outbreaks to regional resources can help cities and counties prepare as the virus spreads. These maps and charts, compiled by Megan Lawson of Headwaters Economics, help give a snapshot* of hospital bed capacity around the West. Please note this information should be considered a jumping-off point for larger discussions about health-care infrastructure, not a resource for people in need of medical care.
The data collected here from the Department of Homeland Security and Commerce Department shows glaring deficiencies in capacity for many regions and unexpected trends regarding where hospital beds are available. For example, on average, rural areas in the West actually have more hospital beds per person than urban areas.
One reason rural areas have maintained this capacity is through a 1997 federal program that provides special funding to keep hospitals running in remote areas. This program has helped some rural hospitals keep their doors open, and yet many parts of the Western US still lack access to health care. That can be especially challenging for people over 65 who often face additional challenges reaching the nearest hospital even as they face higher risk of extended hospitalization and death from COVID-19. In Idaho, Oregon, Colorado and New Mexico, more than 19,000 citizens over the age of 65 live in counties without hospital beds.
In the Seattle area, the first epicenter of the COVID-19 pandemic in the US, King and Snohomish counties combined have just more than 4,900 hospital beds. As of March 18, the two counties have 828 confirmed cases of COVID-19. While not every case will require hospitalization, it’s easy to see how the further spread of the virus could overwhelm medical facilities. This expected shortage is leading King County to build a temporary 200-bed hospital on a soccer field.
In Riverside County, California, the popular retirement community of Palm Springs has issued a shelter-in-place order. The county, home to more than 300,000 people over 65, has 1.1 beds for every 100 senior citizens. In Blaine County, Idaho, where three of the first nine confirmed cases in the state occurred, there is one hospital and 3,800 senior citizens.
Although some rural areas lack local access to hospitals, rural areas as a whole have more hospital beds per person than urban areas in the Western US.
More than 570,000 people in 11 Western states live in counties without hospitals. The majority of those residents are in Idaho, Colorado, New Mexico and Oregon.
We want to hear about your experience dealing with COVID-19. Are hospitals being stretched too thin and is greater capacity needed in your area? Are people finding creative solutions to help care for each other amid this pandemic? Even as we stay home and do our part to stay socially distant, we want to make sure we are connecting as much as possible with the High Country News community. Please consider sharing with us via this secure tip form. You can also share confidential information through this page.
* A note on the data from Headwaters Economics: “This analysis includes general acute-care hospitals and critical access hospitals in the US It does not include military, children’s, women’s, long term care, psychiatric, rehabilitation, or chronic disease facilities that are already being repurposed in some areas.”