Geoff Brooks/Unsplash
This piece was originally published in Undark and appears here as part of our Climate Desk Partnership.
In the past few months, Arinjay Banerjee has gotten an unexpected taste of Internet fame.
Since December, when news of COVID-19 began to shudder across the world, Banerjee—who studies the immune systems of bats at McMaster University in Ontario, Canada—has pivoted his research to focus on SARS-CoV-2, the coronavirus behind the pandemic. Now among the small minority of scientists still regularly doing laboratory experiments, he’s watched his Twitter following grow and his email inbox fill, often with words of encouragement and queries about how and when the virus will be stopped.
But not all the messages Banerjee gets are positive. “You can’t even imagine the range,” he says. Some even include “statements like, ‘You guys have been working with bats, you guys made COVID-19 or SARS-2.’ Or, ‘The reason you have isolated this is because you have it in your lab.'”
These alarmist (and unfounded) accusations are neither new nor exclusive to Banerjee and his colleagues. Many researchers think the negative attention is spurred at least in part by widespread fear of bats—a group of mammals that, in the past several decades, have been repeatedly linked to the emergence of viral diseases, including SARS, MERS, and most recently, COVID-19.
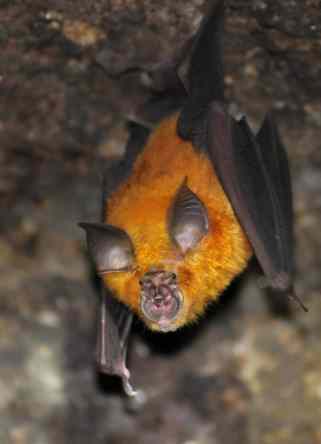
Scientists have suspected for years that bats have struck a strange armistice with some of nature’s deadliest viral killers. Bats that carry infamous pathogens like Ebola, Hendra, Marburg, and Nipah rarely if ever fall ill, or at least show obvious symptoms. Even bats that contract rabies, which is almost always lethal to animals when left untreated, can sometimes emerge from the infection unscathed.
This remarkable resilience has drawn the attention of scientists eager to unravel the secrets of bats’ evolutionary détente with disease—a relationship that could someday yield novel therapies to shore up our own antiviral defenses. But it’s also made bats the targets of loathing among those who consider them little more than stealthy pests teeming with zoonoses, or diseases that can pass from animals to humans. Since the COVID-19 pandemic began, bats have been slandered on social media, targeted for capture or cullings, and even reportedly burned out of roosts—actions that imperil a group of animals vital to ecosystems around the world, Banerjee and other researchers say.
Communicating research findings about bats and viruses without fueling demonization has always been tricky, says Hannah Frank, an evolutionary ecologist at Stanford University. That’s become especially true in the midst of a pandemic with likely zoonotic origins. Through the invasion and destruction of the world’s wild spaces, humans have driven their own exposures to animal pathogens—a cycle that’s only fueled when people act on bat-based fears. But in a moment like this, Frank says, messages like these are easily lost.
Rather than vilifying bats, perhaps humans should consider them our allies in the fight against disease, says David Schneider, a disease ecologist at Stanford University. “I always hope, you know, how can we become more bat-like? That’s the way to do it.”
Communicating research findings about bats and viruses without fueling demonization has always been tricky, says Hannah Frank, an evolutionary ecologist at Stanford University. That’s become especially true in the midst of a pandemic with likely zoonotic origins. Through the invasion and destruction of the world’s wild spaces, humans have driven their own exposures to animal pathogens—a cycle that’s only fueled when people act on bat-based fears. But in a moment like this, Frank says, messages like these are easily lost.
Rather than vilifying bats, perhaps humans should consider them our allies in the fight against disease, says David Schneider, a disease ecologist at Stanford University. “I always hope, you know, how can we become more bat-like? That’s the way to do it.”
The world’s first proper bat likely evolved several tens of millions of years ago, when a lone branch on the mammalian tree converted forelimbs into wings. In the millennia since, bats have splintered into more than 1,400 species—nearly a quarter of Earth’s modern known mammals—and expanded to every continent except for Antarctica. They pollinate plants, disperse seeds, and gobble up insect pests—including bugs like mosquitoes that themselves spread disease. “In many ways, bats are helping us, even though we’re often not helping them,” says Kate Langwig, a disease ecologist and bat conservationist at Virginia Tech.
Given this staggering diversity, it’s important to avoid attributing traits to bats as a whole, says Kristen Lear, a bat conservationist at the University of Georgia. (Some species, Frank points out, haven’t shared a common ancestor in more than 50 million years, making them more evolutionarily distant from each other than humans are from howler monkeys.)
Still, across species, bats seem to accomplish what many other creatures can’t. Winged yet warm-blooded, they’re the only mammals that fly. They age well, in some cases outliving similarly sized mammals like mice by several decades. Several bat species are also resistant to a multitude of ailments, from cancers to infectious fevers that prove devastating to other species, including humans.
Curiously, the apparent lack of sickness in bats doesn’t seem attributable to an immunity to infection. Many of the viruses that have plagued humans in recent decades are found in bats, too—just absent typical symptoms.
Raina Plowright, a disease ecologist at Montana State University, thinks this oddity may be a byproduct of bats’ foray into the skies. Flight is strenuous, ratcheting a bat’s metabolism roughly 15 times above its resting state, sometimes for prolonged periods of nighttime travel. Such exertion takes a toll at even the molecular level, triggering the production of harmful chemicals that can damage the DNA that cells need to function and survive. To cope, bats have apparently evolved sophisticated ways to rein in these destructive substances and stitch battered bits of genetic material back together.
These repair systems appear to be multifunctional, also protecting bats from some of the symptoms of infectious disease, says Michelle Baker, a bat immunologist at the Commonwealth Scientific and Industrial Research Organization, or CSIRO, an Australian federal government agency for scientific research. When most mammals detect a viral invader, they’ll battle it with inflammation, a wildfire-like weapon that helps purge the pathogen from the body but can also wreak havoc on the host’s own tissues. Bats, on the other hand, are able to tamp down these risky responses. Part of this dial-down may overlap with ways they mitigate the detriments of flight; bat cells also seem to have lost some of the machinery required to kick inflammatory systems into gear.

National Park Service
On top of this, laboratory experiments suggest that bats’ bodies may continuously churn out powerful proteins that instruct cells to block parts of the viral life cycle, giving them a “head start” on combating infection, Baker says. Scientists theorize that, with this potent combination of tactics, bats may have hit an immunological sweet spot, mounting a response that keeps invaders at bay without causing unnecessary harm to their own bodies.
To keep their infective skills sharp, viruses that target bats have devised ways to counteract these “unique bat properties,” including evolving powerful molecular tools that allow them to rapidly spread from cell to cell, says Cara Brook, a disease ecologist at the University of California, Berkeley. Accustomed to waging war with the robust defenses of bats, these pathogens can then devastate other species with immune systems that are less resistant to viruses—a bit like a seasoned swordsman parrying with an untrained apprentice.
Bats are tough to study under the best of circumstances: They are both notoriously challenging to monitor in the wild and ill-suited to life in the lab. Many of the conclusions scientists have drawn about bat biology are tentative, and it’s possible some will only apply to the select species that scientists have so far managed to snare, says Vikram Misra, a virologist at the University of Saskatchewan’s Western College of Veterinary Medicine.
It could be, for instance, that viruses do cause illnesses in bats—just not in a way that humans have yet detected, Langwig says: “Just because a bat is flying around happily, doesn’t necessarily mean it’s feeling totally great.”
Other factors beyond immunology play into bat disease dynamics as well. In combination with their longevity and far-ranging flight, the highly social lifestyles of many bats bring them into regular and close contact with each other, offering ample opportunity for infections to spread. All of these complex traits are variables ecologists have only begun to understand.
Aditya Joshi / Wikimedia Commons
Researchers also disagree on whether bats disproportionately harbor viruses with the potential to cause illness in humans. While a 2017 study concluded that bats play host to more zoonoses than other mammals, another analysis published in April found that they were “unexceptional” in their propensity to carry viruses of human concern. Perhaps the preponderance of new virus discoveries in bats, the latter group suggested, could be chalked up to a lack of studies in other animals.
None of that necessarily detracts from the animals’ curious relationship with viruses, says Banerjee, who sees the bat as a biomedical muse for future antiviral treatments. The vast majority of microbes that exist in wildlife, including in bats, pose no threat to humans. But bat-borne infections can still inform a path to peaceful coexistence with viruses and other disease-causing microbes.
In the rare instances where a pathogen does cross the species divide, bats are almost never to blame, Plowright says. Many cultures have a long history of hunting and eating bats and other animals for subsistence. But in recent decades, other human interactions with wild species have escalated to an unprecedented degree as urban areas balloon, forests fragment, and the global wildlife trade—including the sale of exotic luxury meats—booms.
When bat viruses do make the hop to humans, it’s almost always because people have encroached into the territory of animals—not the other way around. Cross-species spillovers, which require a pathogen to be compatible with two often genetically dissimilar hosts in close contact, are extremely uncommon. But by charging into wild spaces, we humans “put ourselves in harm’s way,” says Dan Crowley, a disease ecologist at Montana State University. “If I get drunk and walk in front of a train, I’m not going to blame the train.”
As economic development continues to expand, so too will the number of infectious diseases that plague our population, Plowright says. “We are driving these species to the edge of their ability to survive,” she says. “There’s nothing that’s untouched anymore.”
Pressures like habitat loss or hunting can also drive animals into new environments and cause them undue stress. This in turn hamstrings their immune defenses and increases the likelihood that they’ll shed pathogens into their surroundings. By agitating bats, “we’re just making it much more likely for that perfect storm to happen,” Misra says.
Schneider draws a parallel to Isaac Asimov’s “Hostess,” a 1951 science fiction short story that describes the spread of a mysterious, deadly disease among several alien races that have come to visit Earth. Humans, it turns out, are the source of the infection, which has become a natural and largely unnoticeable part of their existence but swiftly kills extraterrestrial creatures.”We don’t know the silent viruses that we carry,” Schneider says. So perhaps bats shouldn’t be faulted for the company they keep, Langwig says. In fact, they may now need protection more than ever before. In April, the U.S. Fish and Wildlife Service and International Union for the Conservation of Nature both recommended a suspension of fieldwork involving direct interaction with wild bats, out of concern that humans could spread SARS-CoV-2 to North American species. Though a bat version of COVID-19, the disease caused by the new coronavirus, is highly unlikely given these animals’ viral history, bats do suffer their own infectious illnesses, including white-nose syndrome, a fungal disease that has devastated populations across the continent.
Halts to bat research won’t last forever. But Langwig and Lear both worry that even a brief pause in research, including projects focused on bat conservation, could further jeopardize vulnerable species—and, by extension, the ecosystems they support. Bats need to be kept safe, Lear says, especially when they still have so much to teach us.
“There is a huge opportunity there to say, ‘O.K, they can do it, how can we then do it too?'” she says of their ability to coexist with viruses. “So, don’t kill bats. They might actually be the key to learning how to fight these viruses in the future.”