An aerial view shows the Farmer John slaughterhouse, near the Los Angeles River, after 153 workers tested positive for COVID-19, on May 26, 2020 in Vernon, California. David McNew/Getty
This story was originally published by the Food and Environment Reporting Network and is reproduced here as part of the Climate Desk collaboration.
For weeks last spring, as the COVID-19 pandemic spread, the country was gripped by fear of potential food shortages. As speculation arose about widespread meat shortages, Americans started panic buying. Shoppers worried they would contract the virus from food shipped from countries with high infection rates.
These concerns were never borne out. But they distracted from a much more significant crisis underway in the food system: By the time butcher counters were facing an actual meat shortage, scores of workers at the nation’s food and meat processing plants were getting sick and dying of COVID-19. Deemed essential and unable to work from home, hailed as heroes yet forced to share break rooms and lunchrooms in crowded factories, food processing workers quickly became one of the groups hardest hit by the virus.
Reports of outbreaks at these food production plants began last March. By May, they were pouring in. A year later, there have been more than 1,800 outbreaks at food and farm worksites. Nearly 90,000 workers have contracted the virus and 378 have died, based on news reports and public health records aggregated and analyzed by the Food and Environment Reporting Network.
Two-thirds of those cases have been at meatpacking plants, where nearly 30 percent of the roughly 194,000-person national workforce has been infected by the virus and at least 284 workers have died. What’s more, the damage wrought by these hot spots has not been contained to the factory walls. A study released last year linked outbreaks at meatpacking plants to as many as 310,000 COVID-19 cases and 5,200 deaths in surrounding communities—just as of last July.
Media reports and public data about these outbreaks dropped off significantly after the initial surge of worker illness. This dearth of information, and a plateau of new reported cases in the past several months, suggests on its surface that the pandemic’s greatest risk for food and meat processing workers more or less ended last summer.
But what public data show is that instead of abating after the initial surge, the virus in fact returned in waves at dozens of plants last year. A look inside one of those facilities illustrates the risks food processing workers have faced even after the surge of media attention faded, and how an ongoing lack of information, protective gear, and adequate distancing has sickened thousands.
Workers, workplace health and safety experts, and labor advocates warn that even after a year of COVID-19, the conditions in many food processing plants—and the pre-pandemic workplace conditions that had already made food processing dangerous work—remain virtually unchanged, exposing workers to the continued risk of contracting a deadly disease in the course of their workday.
Getting a full picture of the ongoing scope of the COVID-19 crisis for food system workers—or nearly any occupational group—is still impossible, due largely to a lack of disclosure from local and state public health departments and private companies. The federal government, too, has yet to compile or release any rigorous data on worker illness in these sectors. The Centers for Disease Control and Prevention (CDC) has released three reports on the spread of COVID-19 in the food sector, but they relied on voluntary reporting from just 36 states, and only reported worker illnesses as of May 31. The most recent of those reports was released nearly five months ago. As a result, the location of more than half of the outbreaks at food processing facilities remain undisclosed.
Food manufacturing workers are gradually becoming eligible for the COVID-19 vaccine, and thousands have already been vaccinated, offering hope that after a year of devastation, the pandemic may finally be coming to an end. Yet this workforce remains at high risk, despite the meat industry lobby’s assertion that packers’ preventive measures “reversed the pandemic’s trajectory” for workers last spring. And experts say it remains to be seen whether any pandemic-era solutions will fundamentally alter the difficult working conditions in food processing plants.
Meat processing plants anchor rural economies around the country, like in Rogers, Arkansas, population 66,000. The town is home to several poultry processing plants, making it an important node in the so-called chicken belt of the South Central United States. Arkansas itself is a stronghold of food manufacturing, with 49,000 workers in the state’s meat and grain industries. Tyson Foods, the nation’s largest meatpacker, based in Springdale, employs 24,000 workers in the state. There have been more than 860 cases of COVID-19 at five poultry plants in Rogers.
When the first COVID-19 cases were diagnosed at the Tyson-owned Chick-N-Quick poultry plant in Rogers last April, Luis, who has worked for Tyson for a decade, went straight to the plant manager to ask what protections would be provided for him and his colleagues. (Luis is a pseudonym for a worker who requested anonymity for fear of retaliation.)
At the time, he says, there was no hand sanitizer or masks at the facility and no plan for how to quarantine workers who were exposed to the virus. Luis took two weeks off using his own vacation days, hoping to return to a safer workplace.
But it was early May before workers were given cloth masks, he says, and several more weeks until they got surgical masks. Even then, he says, masking was inconsistent because wearing them wasn’t required. As the months passed, workers were largely in the dark about how many cases there had been at the plant.
“Communication was barely given,” Luis says through a translator. In a once-a-month meeting, workers heard “that the situation was in control, that there were not many cases going on, and if the cases were coming, it was not because people were getting infected at the plant—it was because those workers got it outside the plant”—an assertion the industry and elected officials have made repeatedly about food worker illness in the past year.
Yet cases were ticking up at the Chick-N-Quick plant all spring. News reports and data from the Arkansas public health department show that there were more than 20 worker cases by mid-June.
For several months last fall, it seemed the Chick-N-Quick outbreak had subsided. But then, in late December, the plant suddenly reappeared in the state public health department’s biweekly reports on occupational COVID-19 outbreaks—and with a shocking leap in new cases. In early January, nearly 130 worker illnesses were reported at the facility, which employs 917 workers.
It’s difficult to know exactly when workplace outbreaks begin and end, in part because states and counties have no standard process for reporting workplace outbreak data. But an analysis of state data shows that the Chick-N-Quick facility was one of more than 50 meatpacking and food processing plants that had a second wave of infections after a gap of at least two months. More than 6,700 worker cases and 22 worker deaths are linked to these repeat outbreaks.
These plants are located mostly in states or counties that have been reporting regularly on cases and workplace outbreaks of Covid-19, like Oregon, Colorado, and Arkansas. Few other states are reporting any data about worker illnesses and workplace outbreaks, making it impossible to know the full scope of the pandemic in food processing plants.
Map by Leah Douglas, FERN
The Colorado health department confirmed that there have been multiple outbreaks at nine plants in the state, and the Los Angeles County health department confirmed one plant with multiple outbreaks. The Arkansas and Oregon health departments declined to provide further details about multiple outbreaks that show up in their health data, and the Kansas health department did not respond to a request for comment. In other states, media reports confirmed multiple outbreaks at the mapped facilities.
Experts say a range of factors could contribute to a plant experiencing repeated waves of COVID-19 infections. Workers may have lacked sufficient protective gear or the space to social distance, or were inadequately trained on precautionary measures. Luis’ experience of poor communication at the Chick-N-Quick plant has been typical at many food and farm workplaces during the pandemic, says Suzanne Adely, co-director of the Food Chain Workers Alliance, a worker advocacy group.
“Our members [were] reporting, ‘They’re not giving us information, we don’t know what to do, the information that’s there isn’t even in our language. We don’t know what’s going on,’ ” Adely says.
At meatpacking plants in Nebraska, some workers have been told by managers not to take photos of the interior of plants or disclose the results of their own Covid-19 tests to co-workers, says Dr. Athena Ramos, an assistant professor at the University of Nebraska Medical Center.
“Workers are fearful of speaking up because of some of the repercussions they think they’ll experience,” she says. “That is a major concern.”
In some cases, it’s impossible to know how the virus is spreading in a plant because of a lack of transparency from the industry, says Dr. Fredric Gerr, a professor of occupational and environmental health at the University of Iowa.
“It’s remarkable the extent to which there are barriers for knowing what is going on inside these facilities,” he says.
In the case of the Chick-N-Quick plant, Luis says the virus appeared to subside only because workers were being tested inconsistently. Each week at the plant, he says, 20 workers are randomly chosen for testing. But workers outside of that random pool—even if they have symptoms consistent with COVID-19—can’t get reliably tested, Luis says. He calls the testing protocol a “gambling game,” in which the company wants to avoid testing a broader swath of workers because “everyone will be sent home.”
“The company is basically playing with our health,” he says.
This account is inconsistent with Tyson’s public statements about worker testing. The company has said for months that it is testing thousands of its employees each week to monitor for new outbreaks. Yet since last spring, when the company made public testing results from 18 of its plants, it has not released any more information on how many of its workers have contracted COVID-19. Relying on government health data and media reports, FERN has traced more than 12,500 cases and 39 deaths to outbreaks at 57 Tyson plants.
In response to emailed questions, Tyson spokesperson Derek Burleson said that the company made hand sanitizer and masks available to workers last April and notifies workers if they come in close contact with a colleague who tested positive for COVID-19. Burleson said the company’s testing strategy, which includes “using random testing as a tool to find the virus, testing thousands of workers a week, both symptomatic and asymptomatic,” is consistent with CDC guidance.
Experts say that workers should have access to testing at plants if they’re experiencing symptoms, and that testing should be conducted regularly for all workers. A rigorous testing program should continue even as vaccines are rolled out to the workforce, says Dr. Robert Harrison, a physician and director of the Occupational Health Services Program at the University of California, San Francisco.
“Testing is a crucial tool for monitoring the health of workers as long as they remain at some risk of COVID infection,” he says. “We should not let up. We should remain vigilant until we see that vaccination has put a stop to transmission and that the genetic mutation or variants do not require a change in our vaccine plan.”
The CDC is currently reviewing its guidance on workplace testing, according to a March memo, as part of an agency-wide review of Covid-19 protocols released during the Trump administration.
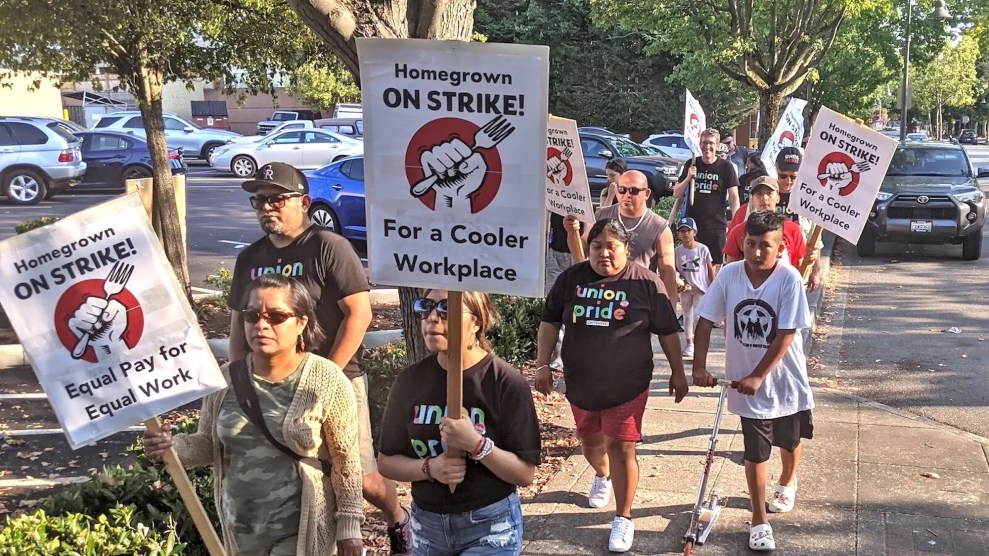
Meanwhile, Adely says that despite thousands of illnesses and hundreds of deaths, the pandemic hasn’t changed much about the working conditions at these plants. Workers may have access to masks now, she says, “but in terms of the actual conditions that prevent social distancing or the power dynamics that prevent workers from being able to speak up, that still hasn’t changed. That’s the context in which outbreaks are allowed to happen.”
At the Chick-N-Quick plant, despite months of worker cases, Luis says it is still difficult for workers to adequately distance. “Everything is small: the lunch break (room), the bathrooms, the hallways,” he says. “It’s impossible to not have people caught in small spaces.”
A video of a tour of the facility from June 2020 shows plastic barriers had been installed at tables in the worker cafeteria to prevent the spread of COVID-19. But the chairs around the tables were bolted to the floor, just inches from one another.
Similar conditions have contributed to an outbreak at a Los Angeles County sausage factory owned by Smithfield Foods, where nearly 800 workers have contracted COVID-19 and five have died. The outbreak is one of the largest and deadliest at any meatpacking plant in the country. The biggest jump in new cases at the plant occurred not last spring but this January, when there were more than 300 new worker infections, county data show.
The meat industry, however, asserts new worker cases have fallen nationally, as a result of employers’ efforts to protect workers from COVID-19. The North American Meat Institute (NAMI), a trade organization whose members include Smithfield, Tyson, and JBS, says meatpackers have spent over $1.5 billion dollars on worker protections during the pandemic.
“The implementation of the protocols that have been put in place without a doubt have reduced the caseload,” says Julie Anna Potts, NAMI’s CEO and president. Using FERN’s data on meatpacking worker illness, the group has calculated that worker cases are 98 percent lower now than last May, Potts says.
Yet the industry also refuses to disclose internal data on how many workers have contracted or died of COVID-19, presenting a major barrier to understanding the spread of the virus. Last July, Tyson, Smithfield, JBS, and Cargill declined to provide worker illness data to Sens. Elizabeth Warren and Cory Booker as part of an investigation into the industry’s handling of the pandemic. In February, the House Subcommittee on the Coronavirus Crisis also requested this data; the results of that investigation have not been made public.
Potts says that NAMI doesn’t collect worker illness data from its member companies for confidentiality reasons.
Public data on occupational outbreaks are thin in part because private businesses have pressured elected officials and public health agencies not to report worker illnesses and deaths.
In Iowa, Gov. Kim Reynolds announced in late May that the state would disclose outbreaks at meatpacking plants only if the information was requested by a reporter, in part to give industry “the opportunity to take the lead” in notifying the community of an outbreak. At the time, food system workers accounted for one-third of all of Iowa’s COVID-19 cases. The state is still not publicly reporting meatpacking plant outbreaks or worker cases.
In Nebraska, Gov. Pete Ricketts last May stopped health officials from publicly reporting cases at meatpacking plants even as plant workers accounted for nearly one in six cases of COVID-19 in the state. Ricketts recommended that local health officials get permission from the industry before releasing case counts, and the industry declined to share case counts because, it said, of privacy concerns. These policies are still in place.
The Arkansas public health department last summer began releasing occupational illness reports that identified specific plants with COVID-19 outbreaks. But in September, the department changed its reporting practices without explanation and now identifies these outbreaks by broad sector in twice-weekly reports.
North Carolina was planning to publish data on workplaces with COVID-19 outbreaks last spring but never followed through, in part because local health officials were concerned that meatpacking companies would balk at public reporting of their outbreaks and potentially decline to participate in worker testing or other public health efforts in the future. Wisconsin, too, considered releasing outbreak data twice last year, but changed course after lobbying from chambers of commerce and other business interests.
A few states are releasing only cumulative totals of worker illnesses and outbreaks in the food and agriculture sector. Others are not collecting this data at all, or have declined to share the information upon request. As a result, the locations of more than half of the nearly 600 outbreaks at meatpacking plants—and around 60 percent of the outbreaks at all food system workplaces—remain undisclosed and are not included in FERN’s map of food system outbreaks.
Advocates have argued that this lack of data poses a serious public health risk. Magaly Licolli, an organizer with the Arkansas-based poultry worker advocacy group Venceremos, says that the state department of health’s failure to release worker illness data by specific facility has contributed to the continued outbreak at the Chick-N-Quick plant.
“Instead of making it more transparent, they’re making it worse,” she says. “There is a huge outbreak in the Chick-N-Quick plant, and no one is talking about it. They have normalized it, and it’s very concerning.”
As the pandemic enters its second year, experts say vaccines are the key to protecting this embattled workforce. A successful vaccination campaign will require “educating workers about the vaccine and making the vaccine available at work, making it very easy for individuals to make the decision to get vaccinated,” says the University of Nebraska’s Athena Ramos.
The issue of vaccine access and distribution has united the meat industry and worker unions, which all agree that food system workers have not been adequately prioritized to receive vaccinations and that the federal government should move essential workers into higher-priority categories.
Many states have veered away from the CDC’s Advisory Committee on Immunization Practices recommendation to place food and agriculture workers in Phase 1b, the second priority group for vaccination. Food processing and meatpacking workers are now eligible for vaccination in a majority of states, according to a review of health agencies and news reports by FERN. But there are notable exceptions—like Florida, home to thousands of farmworkers—and several northeastern states.
“Vaccine access for essential food workers in these plants will help to prevent the deadly outbreaks we saw last year and keep our food supply secure as this crisis continues,” said Marc Perrone, the international president of United Food and Commercial Workers, which represents meatpacking workers, in a statement. “UFCW is calling on governors and CEOs in every state to act swiftly to ensure every essential food worker in America has access to the vaccine. Lives are on the line, and we cannot wait any longer.”
But vaccines are just one tool to mitigate the spread of COVID-19 in these plants, experts say, because not all workers will be vaccinated in the near term and because the industry has a high turnover rate. Employers should be ensuring that workers have access to robust testing, protective equipment, and paid leave, and taking preventive measures like filtering the air in plants and allowing workers to adequately distance.
Labor and workplace safety advocates are still hoping the Occupational Safety and Health Administration will release an emergency temporary standard, which would create enforceable rules for how employers must protect their workers from COVID-19. On his first day in office, President Biden directed OSHA to review whether such a standard should be implemented. OSHA also recently announced that it would begin prioritizing inspections where workers are at high risk of contracting Covid-19, including meat and poultry plants.
To ensure that these federal measures are implemented successfully, workers need to be involved, says Adely.
“Workers need the power to be able to determine the conditions that affect their health and safety on a daily basis,” she says. “Workers just need more of a say about how these inspections and enforcements are done and how, then, the recommendations are implemented in the workplace.”
And regulators and the public need better access to information about worker illness to ensure the industry’s efforts are most effective, says the University of Iowa’s Fredric Gerr.
“Good surveillance of COVID in industry would be powerfully useful,” he says. “Knowing the scope or extent of the problem is invariably the first step in creating a prevention strategy.”