When Phoebe McNeece showed up at the community health center in her small town in Southeast Iowa a few days after New Years 2012, the last thing she wanted to hear was that she was pregnant. Uninsured and unable to afford her medication, she was becoming increasingly anxious and depressed. She was struggling to keep her job, which meant she was behind on the mortgage on the little house she’d bought three years prior. And now, here she was, telling this doctor that she really hoped that home test she had taken was just a false positive.
A few minutes later, he came back into the exam room—”Congratulations, you’re pregnant!” he said. Phoebe broke down in tears, the sobs wracking her body.
“Stop crying, stop crying,” Phoebe remembers the doctor saying, his hand on her shoulder. “This is a good thing. This is what you were put on earth to do.”

The War on Women Is Over—and Women Lost
Phoebe went through with the pregnancy and is a 31-year-old single mother to her son, a rambunctious four-year-old. She doesn’t go to that clinic anymore—that encounter, she says, made her feel like “an incubator instead of my own person”—opting instead to get her reproductive health care, from birth control to annual exams, at the Planned Parenthood clinic in Burlington, Iowa, five minutes from where she lives.
On a muggy June evening, we meet at Phoebe’s friend Laura’s house, along with a third friend, Alexandra—both also longtime Planned Parenthood patients. After the 2016 election, they each felt compelled to get more involved in politics and met through an anti-Trump Facebook group. Alex and Phoebe’s sons run circles in the living room in between bouts of Nintendo, while Laura’s fiancé tries to keep their ten-month old out of the food spread. The three women talk about local politics with the authority you’d expect from Beltway powerbrokers—from rehashing their representatives’ positions on everything from collective bargaining rights to schools to reviewing election filing deadlines, as Alex and their friend Ryan are considering a run for local office.
They have studied up in part because their state, which became a Republican trifecta in November, is taking away the care that they and thousands of other women have come to depend on by defunding Planned Parenthood. “Iowa just flipped to being a completely different state from what I remember,” Phoebe says. “When the governor signed the bill to defund Planned Parenthood, we had to focus on that.”
Iowa is now just a few steps ahead of the Trump administration. The president and congressional Republicans are in the process of trying to pull Medicaid funds from the women’s health care provider through virtually every Washington mechanism available: the Administration’s budget proposal, separate legislation sponsored by Iowa’s own Sen. Joni Ernst, and most imminently, a repeal bill that would undo Obamacare and replace it later, which is slated for a vote in the coming weeks.
“President Trump ran on this issue. I’ve heard him speak about it. The crowds of 10,000, 20,000 would cheer,” said Iowa state Sen. Jason Schultz in February of his state’s Planned Parenthood defunding. “This is going to be a good move for Iowa, to be one step ahead of what’s happening as a nationwide trend…a tide coming in that’s moving in one direction.”
That tide, health care experts warn, would gut family planning care well beyond the Hawkeye state.
“Planned Parenthood sees over 2.3 million patients a year. They provide a lot of the ongoing contraception and reproductive health care for a lot of women, especially women in rural areas,” says Dr. Hal Lawrence, an OB/GYN and the executive vice president of the American College of Obstetricians and Gynecologists. “If they lost their Medicaid dollars, it would be dramatic, and sadly, it’d be catastrophic.”
In May, then-Iowa Gov. Terry Branstad signed a new budget bill that rejected $3 million in federal Medicaid dollars for the Iowa Family Planning Network (IFPN) waiver—partial insurance for low-income patients that covers reproductive care—and replaced it with a state-run family planning program that forbids recipients from using it for care at providers, like Planned Parenthood, that also offer abortions. (Federal money already can’t fund most abortions, thanks to the 1976 Hyde Amendment.) As a result of this new budget, on July 1—the day this new law went into effect—4 of Iowa’s 12 Planned Parenthood clinics, including Phoebe’s and the other two near her in Southeast Iowa, closed, leaving the bottom third of the state without a Planned Parenthood clinic.
Burlington’s clinic served 96 percent of the county’s patients like Phoebe—those who are on publicly funded insurance for family planning care. The other three, in Keokuk, Sioux City, and Quad Cities, served 92 percent, 80 percent, and about 37 percent respectively. Other providers that are now excluded are UnityPoint Health and the University of Iowa hospitals and clinics, because both offer medically-necessary abortions, including those when a serious fetal anomaly is discovered—a type of abortion not exempted in the legislative calculus for who gets kicked off the state’s family planning program.
This means that at least 15,000 patients now need new places to go for family planning care. Hardest-hit are low-income patients, particularly those in Iowa’s rural Southeast, where hardly any other reproductive health care providers will take their insurance: As of this writing, the state’s new family planning program provider list includes no OB/GYN specialty providers in Burlington, Keokuk or in neighboring Louisa and Muscatine Counties. Three providers are listed in Quad Cities—two are midwives.
Some Iowa lawmakers raised the alarm about the lack of viable options before the bill passed. In a January hearing, democratic state Sen. Janet Petersen asked her Republican colleague Sen. Jeff Elders to discuss alternatives in his district that could offer reproductive health care; he could not name any, replying “more access” before shutting off his microphone.
Sen. Petersen followed up with multiple senators for more specifics on alternatives, yet still nothing. She concluded: “Finding a provider to give you a pap smear shouldn’t be rocket science.”
Officials eventually released several lists of proposed alternatives. An initial list offered by a state senator to a reporter included a dentist, a school nurse, and a homeless shelter. A different list from the Iowa health department obtained by the Des Moines Register in May had 219 proposed alternative providers; many were duplicates and dozens are run by the Catholic Mercy Health Network, which does not offer intrauterine devices or other long-acting contraceptives, and will only prescribe oral birth control to treat “medical conditions”—doublespeak meaning they won’t offer voluntary contraception. As of July 17, the Iowa health department’s list of providers had only 73 approved OB/GYN providers for the entire state. More than a third were duplicates. (When I asked the Iowa health department whether they anticipated that these OB/GYN providers would be sufficient to meet the reproductive health care needs of patients on the family planning program, they declined to answer.)

The replacement plan is also a fiscal double whammy: Iowa is giving up millions in federal money and plugging the hole with state taxpayer dollars—while facing a $117 million budget shortfall. Yet Republican lawmakers avoided getting into these thorny money questions while advancing their plan. Said one senator: “We are committed to getting the money from somewhere.” Before the proposal was folded into an appropriations bill, its main sponsor, state Sen. Amy Sinclair, said, “This is a policy bill strictly. I do not deal with the financial aspects.”
As Democratic Sen. Matt McCoy summed this up on the Senate floor: “So we’re gutting a program that is currently federally-funded and replacing it with an unspecified amount of money from an unspecified place,” he said. “That scares me.”
Iowa lawmakers had floated an early proposal to fund the program by redirecting money away from a different federal allotment—the Social Services Block Grant—that, in Iowa, funds disabled services,foster care, and adoption, among other services. The proposal garnered criticism for taking money away from child welfare programs and was ultimately dropped: All $3.4 million in funding for the new program now comes from state general funds.
The Quad Cities Planned Parenthood started double booking patients for the first few weeks after the Governor signed the bill that shut them down. When I arrive at the clinic on a June morning, a large sign is slung across the brick façade of the anti-abortion clinic across the street, facing Planned Parenthood’s parking lot: “If you have taken the ABORTION PILL, it is possible to REVERSE this decision. Stop in and see us.”

Trump Brought the War on Women Mainstream in His First 100 Days
Angela Rodriguez-Finch, this Planned Parenthood’s center manager, gives me a tour. One hallway wall is covered in neon post-its and postcard messages sent to the clinic since the governor signed the defunding provision by grateful patients and supporters. What used to be the health educator’s office is dark and empty; the woman who worked there used to provide sexual health education and outreach at schools in the Quad Cities, but with the clinic’s imminent closure, she’s been reassigned. The shelves where patient charts used to be filed are bare, with all the folders now stacked in cardboard boxes, waiting to be put into storage until the clinic’s patients can find new providers.
Most of them haven’t. “Patients aren’t saying, ‘Oh, send my records here,'” explained Angela Axdahl, the local Planned Parenthood affiliate’s regional director of health services who oversaw all three of the Southeast’s now-closed clinics and their 10,000 patients. “They’re saying ‘Where am I going to go?’”
That’s in part because these areas in particular have a dearth of providers—Burlington, for instance, is in Des Moines county, which the US health department has designated a health provider shortage area. But it’s also because of something less tangible, but no less important: for many women, Planned Parenthood offers no-judgments care in places where sexual health care often comes with a lot of dogma attached.
Phoebe’s friend Alex, who grew up as a Mormon in Burlington, recalls that when she was facing her own unplanned pregnancy, she knew she wanted to keep the baby but was terrified of her community’s judgment. Her concerns were justified: The bishop disciplined her with a 6-month “disfellowship,” or suspension, from the church.
“Being an unwed mother as a conservative Mormon was just the worst thing I could have ever done,” Alex says. “Planned Parenthood was the first place that made me feel like ‘I’m going to be a mom and I’m going to be okay.’ There was no judgment. You don’t get that in a doctor’s office in a conservative area.”

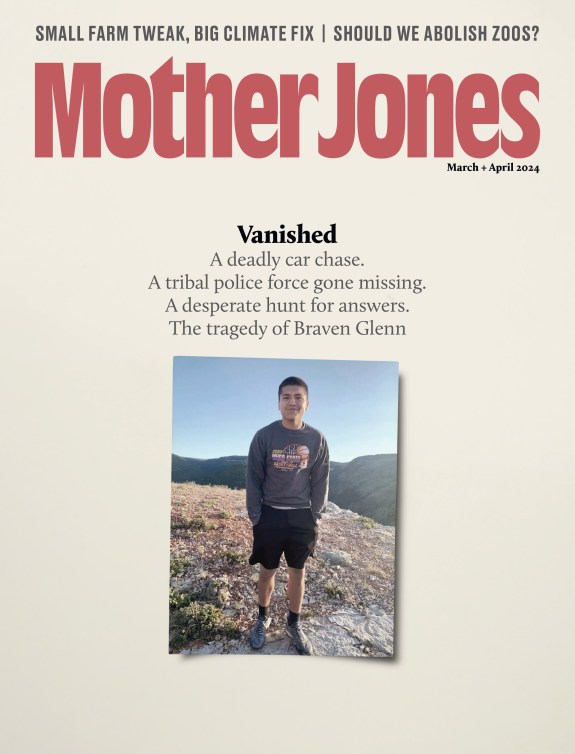
L to R: Laura Blanchard, Phoebe McNeece, Alexandra Rucinski
Alyssa Schukar
I heard many more stories like this one: Laura tells me about seeking care from an OB/GYN and fertility specialist who advised that her best chances for getting pregnant were as soon as possible following surgery for her Stage 4 endometriosis. Laura told him she and her fiancé were on board, and would postpone planning the big wedding they wanted. This was more important. The doctor responded that he would not give her fertility treatment if she wasn’t married.
At the Quad Cities clinic, one of the nurses tells me that in her four years working there, she’s had “a handful” of patients who tried to return to their regular provider after coming to Planned Parenthood for an abortion, only to learn that this new event in their medical history meant their providers now refused to treat them. A clinician adds that several of her patients’ regular providers did not diagnose their sexually transmitted diseases. “I think a lot of clinicians are afraid to mention ‘Could this be a sexually transmitted infection?’ or to say ‘We’re going to screen you’ because of the stigma with that,” she says.
Just as women across America rushed to get IUDs following Trump’s election, fearful that Obamacare’s contraceptive mandate would be repealed (as of this writing, federal regulators are reviewing a Trump administration proposal to do just that), so too across Iowa, many patients made plans for future care that, by design, won’t involve the doctor’s office. Some came in for IUDs or Nexplanons, Axdahl explains, while others replaced their long-acting contraceptives early, if their insurance permitted it, so they have a few more years before needing a replacement.
With their clinic now closed, Alex and Phoebe, who are both on Medicaid, have also come up with alternative plans predicated on avoiding traditional medical providers. Alex has a prescription for a year’s worth of her Depo-Provera birth control shot, which a relative who is a nurse will administer every three months. Phoebe’s plan is no plan at all: She worries her old car wouldn’t survive the four hours round trip to the next nearest Planned Parenthood, in Iowa City, and as a sexual assault survivor, she’s wary of new providers and prefers to see a female doctor. So for now, she intends to skip reproductive care altogether and hope that, when her IUD expires two years from now, the political winds will have shifted.
This is not surprising. “There’s a lot of evidence of what happens when a hospital or clinic closes in a community,” says Dr. Georges Benjamin, the executive director of the American Public Health Association (APHA). “Those patients don’t get easily redistributed. We know that. This is not theoretical. Those patients often end up kind of wandering.”
Iowa officials appear to be oblivious to these kinds of realities. During a Senate floor debate, lawmakers promised that other providers would easily pick up the slack to provide equal care. “Women will not go without exams or care or screening,” said one state Senator. “They will just receive those services where they live.”
But it’s not that simple. When we speak in mid-June, Ron Kemp, the CEO of Community Health Centers of Southeastern Iowa, says he’s been trying to make plans to absorb some of Planned Parenthood patients, but he doesn’t know how many to expect. Historically, patients were encouraged to go to Planned Parenthood for reproductive health care needs—particularly long-acting reversible contraception—in part because it was more cost-effective. Kemp says his centers have purchased a small number of LARCs and are training staff on how to insert less-expensive hormonal implants, like the Nexplanon. They’re also considering options for how to handle certain services they can’t provide in-house. “We have providers who do provide some women’s health services. But not the full spectrum of women’s health care,” Kemp says. “It’s a suspicion on my part that some of the patients will have a struggle being comfortable. They had long-term relationships with providers at Planned Parenthood. Those kind of situations don’t easily change for people.”

If Trump Gets His Way, These Will Be the First Places to Ban Abortion
Still, Iowa officials maintain that the new family-planning program will be just as good as the old one. Trump’s Department of Health and Human Services seems to agree. The department reportedly gave Iowa permission to fast-track its defunding of Planned Parenthood, in violation of the agreement the state made with Obama’s HHS that required at least six months before the old program could be terminated. (Iowa ended it’s Medicaid-funded program just a month and a half after the governor signed the budget defunding Planned Parenthood.)
“We had conversations with our federal partners,” says Julie Allison, a bureau chief at the Iowa Department of Health Services when I ask about the six-month rule. “You know, when they made that rule, it’s for really when they close a program. Because we’re replicating the program, we’re not required to do the phase out.” The HHS Center for Medicare and Medicaid Services did not respond to requests for comment on this.
Iowa lawmakers could have looked south to see the likely long-term effects of their new family planning effort. Between 2011 and 2013, Texas Republicans rejected millions in federal Medicaid funding to undermine Planned Parenthood and other abortion providers. As a result, 82 of the state’s women’s health clinics closed, about a third of them belonging to Planned Parenthood. In the next three years, nearly 50,000 fewer women received reproductive health care through the new state-run program. Medicaid claims for long-acting contraceptives declined by 35 percent while Medicaid-covered childbirths increased by 27 percent, and maternal mortality rates doubled.
Iowa’s mostly Medicaid-funded family planning program, on the other hand, has been around for a decade—and in that time has seen a net savings of more than $265 million in Medicaid spending, thanks in part to more contraceptive access and fewer childbirths, as well as a 32 percent reduction in the abortion rate.
In an extraordinary move in June, Iowa’s Council on Human Services, a group of advisers to the health department appointed by the governor, went rogue, and voted to reject the health department rules that would set up the new family planning program required by the law. But within two days, the attorney general’s office informed them that rejecting department rules would not undo the legislation. The council begrudgingly approved the program while continuing to voice their concerns. “There are some people like me who are adamantly anti-abortion, and therefore adamantly in favor of accessibility to birth control,” said council chairman Mark Anderson, a Lutheran minister. “I am deeply concerned.”
If Planned Parenthood is defunded at the federal level, the entire country will face a situation similar to the one in Iowa: ideology informing health care in spite of the facts. Approximately 1.5 million patients who currently get care at Planned Parenthood through federal funding would have to find new providers. 2015 data from the Guttmacher Institute (the last year for which data is available) shows that if all Planned Parenthood clinics were to close, community health clinics around the country would have to double their caseloads to fill the void, to the tune of about 1.9 million extra people. The predictions are so dire that two Republican senators, Alaska’s Sen. Lisa Murkowski and Maine’s Sen. Susan Collins, have broken with their party and vowed to vote against stripping Medicaid funds from Planned Parenthood. Still, most of their Republican colleagues insist that community health centers will easily pick up the slack.
“This is one of the myths that’s being passed around by the proponents of this bill in Congress—that there are all these programs that can pick [Planned Parenthood’s] patients up” says Dr. Benjamin of the APHA. “There are not.” Many of those programs are already stretched to the limit, Benjamin says, adding that many community health centers already increased their patient base following Obamacare’s Medicaid expansion. “There’s no question that there will be an enormous void in women’s services in many communities.”

Trump’s Pick for Health Secretary Has Spent Years Trying to Limit Access to Contraception
In May, Alex, Phoebe, and Laura organized a march in Burlington to protest the closing of their local clinic. Alex led the group of more than 100 down the winding cobblestones of “Snake’s Alley,” the (somewhat-contested) “crookedest street in the world,” to the plaza in front of Burlington’s miniature replica of the Statue of Liberty.
Women took turns at the pink megaphone to share stories of how Planned Parenthood helped them. Alex spoke about the Burlington clinic’s support when she was scared about her pregnancy, and Laura described her experience of getting confidential care at Planned Parenthood after being sexually assaulted in college.
Phoebe wasn’t planning to speak, but at the last minute, she decided to share her experience at the community health center she went to five years ago—the one that will now be her main alternative with the Burlington clinic closed. “It’s way more nuanced than, ‘Planned Parenthood performs abortions, so we need to close them down,'” Phoebe says. “I really hope we are not a bellwether for the country. I hope the rest of the country says. ‘We don’t want any part of what Iowa is doing right now.'”